Preventing Medicine Shortages: Governments are Saying it’s Time for Transparency
Continuing legislative developments in the US and new government strategies in the UK and EU show that pressure for pharma supply chain visibility is growing.
It’s a new year, but the same pressures on pharma supply chains remain – and the increasingly similar responses from governments across the globe.
In the US, momentum continues towards regulation. Last year, Michigan Senator Gary Peters introduced the Mapping America’s Pharmaceutical Supply Act into the US Senate. The Act aims to boost the visibility of the pharma supply chain to identify reliance on foreign manufacturers and “chokepoints” in the supply.
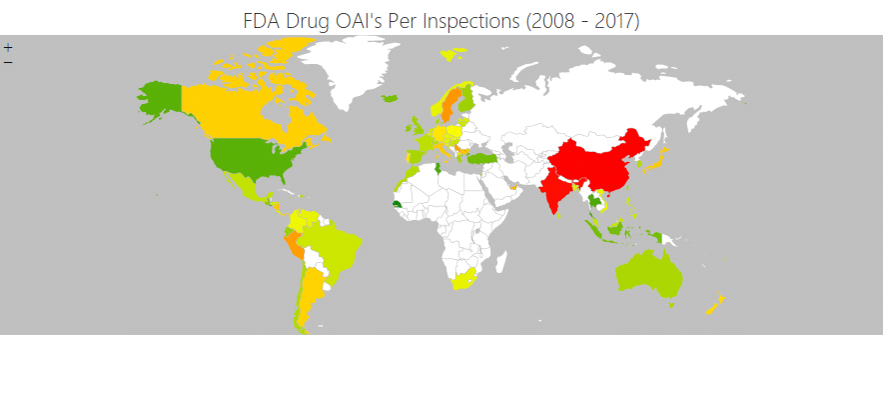
As our guide to MAPS explains, the Act would require the Department of Health and Human Services (HHS) to establish a federal database to map the origin of each drug, including the location of manufacturing facilities and associated inspections and risks, and use this to identify risks to the supply chain and boost resiliency.
The bill is currently working its way through the Senate, having been referred to the Committee on Health, Education, Labor, and Pensions.
A New Legal Boost for Supply Chain Transparency
In the meantime, in January, the US House of Representatives saw its own version of the MAPS Act – again enjoying bilateral support being introduced by the Democrat representative for California Doris Matsui, and Indiana Republican Larry Bucshon. The content is largely the same, with a requirement for the HHS to establish a list of essential drugs and APIs and provide visibility of pharma supply chains.
“The [HHS], in coordination with the heads of other relevant agencies, shall support efforts, including through public-private partnerships, to map the entire United States pharmaceutical supply chain, from inception to distribution,” the bill mandates. The information should then be used to identify supply chain vulnerabilities “and other national security threats”.
As Matsui herself explained: “Recent drug shortages across the nation have made it acutely clear that we need to improve our ability to anticipate, identify, and respond to cracks in the system.
“The lack of end-to-end visibility into every step of our pharmaceutical supply chain means we don’t know the extent of our reliance on foreign agents for key drug ingredients, or how a natural disaster would impact the drug supply. The MAPS Act is a crucial step to provide us with a comprehensive roadmap. By increasing transparency, we can bolster the weaknesses in our supply chain and prevent future public health emergencies.”
Like the Senate bill, the House’s effort is also winning outside praise, with the American Hospital Association (AHA) lending its support.
“The AHA appreciates the efforts of Representatives Matsui and Bucshon to address the chronic and increasing drug shortages hospitals, health systems and patients are facing across the country,” said Lisa Kidder Hrobsky, AHA senior vice president for advocacy and political affairs.
A Wider Move to Supply Chain Resilience
The MAPS Act is not the only way the US legislature and government are taking a more active approach to boosting pharma supply chain resiliency.
As noted previously, another of Senator Peters’ bills is the Rolling Active Pharmaceutical Ingredient and Drug (RAPID) Reserve Act. Also focused on the HHS, it would require the department to contract OECD generic drug manufacturers to build reserves of critical drugs and prioritise domestic producers for federal contracts.
January also saw Florida become the first US state to gain FDA approval to import cheaper drugs from Canada to tackle surging prices in the US. While it’s the result of a law passed more than two decades ago, pressure has grown in recent years to see the freedom used.
President Biden’s executive order in 2021 called on the FDA to work on such import plans.
The FDA approval came despite opposition from the Pharmaceutical Research and Manufacturers of America (PhRMA) and the Partnership for Safe Medicines, which say imports of unapproved drugs from Canada pose a danger to public health.
The FDA, however, said it was committed to working with states on such proposals so long as they “demonstrate the programs would result in significant cost savings to consumers without adding risk of exposure to unsafe or ineffective drugs”.
It’s not just the US, either, however.
A New UK Pharma Supply Chain Strategy
Like the US, the UK continues to suffer frequent supply chain shortages for essential medicines. Far from getting better since the end of the pandemic, they’ve worsened.
According to the British Generic Manufacturers Association, shortages have doubled since the start of 2022. Community Pharmacy England chief executive Janet Morrison said the shortages were unprecedented.
“Pharmacy teams have been struggling to get hold of prescription medicines for many months, but the problem is now worse than ever,” she told The Guardian.
Just a few days later, the government published its new strategy to protect critical imports and supply chains.
“The events of recent years have shown the world that we cannot afford to take for granted the resilience of the global supply chains which we rely on for our critical imports,” the foreword notes. “The COVID-19 pandemic, Russia’s illegal invasion of Ukraine, and disruption to shipping routes have all demonstrated the potential impact of global events on the reliable flow of vital goods.”
Its response is the strategy: The UK’s “first overarching strategy focussing on reliable access to the goods we need now and in the future”.
Among those it considers critical goods are those whose disruption would significantly impact essential services, the economy, national security or “life”, which includes “medicines and delivery of patient care”.
The health sector is also one of those considered as critical national infrastructure.
Promoting UK Supply Chain Transparency
The strategy notes that supply chain resilience is “a shared objective” for both government and suppliers, requiring dialogue between all parties. It also notes a range of measures already in place to promote transparency and resilience.
These include requirements for medicine manufacturers to report shortages to the Department for Health and Social Care (DHSC) and the National Supply Disruption Response established as a central point of contact for healthcare providers that have exhausted other options to maintain supply.
“Supply chain resilience is also an important consideration of awarding contracts to suppliers when procuring medicines and medical products, with a focus on developing available buffer stocks on British soil, such as in the case of generic medicines or high-use clinical consumables,” it adds.
In other sectors, it notes, the government has directly intervened in markets to ensure protection against profound shocks – requiring specific sectors such as defence to maintain stockpiles of critical goods for national security.
That is currently reserved for the most serious case, but the next steps in the government strategy will include a “framework to formalise government approach to supply chain shocks, setting out how government will work with business to ensure a coordinated response”.
EU Efforts for Supply Chain Resilience
What that framework will look like in the end is unclear. Different governments take different approaches, and there is no single solution to supply chain issues. Indeed, individual governments are – as in the US – employing a variety of strategies to keep essential medicines available and affordable.
It’s a similar story in the EU. Its recommendations published last summer to prevent antibiotics shortages included boosting production, monitoring supply and demand and promoting “prudent use” among the public. In December, meanwhile, the European Medicines Agency published its list of 260 critical drugs, including vaccines, painkillers and asthma medicines, which the European medicines regulatory network is to prioritise in EU-wide actions to strengthen their supply chain.
As the Financial Times reports, “proposals could include measures to encourage companies to stockpile products and diversify suppliers, investment incentives for new manufacturing plants in the EU and the introduction of joint procurement protocols as the bloc did with Covid-19 vaccines”.
The First Step Towards Improved Supply Chain Visibility
Whatever and wherever action is taken, however, supply chain transparency is an essential ingredient and a necessary first step.
Whether that comes directly through MAPS-type regulation or indirectly, in response to regulatory demands to identify and address vulnerabilities, will, in the end, make little difference.
It is the pharma businesses who are best placed to identify the criticalities and vulnerabilities that must be addressed to ensure resilience – and it is they who will face irresistible pressure to do so. It’s through technology such as SCAIR®, which helps identify choke points and common dependencies on APIs or manufacturing sources, that they can do so.
We can’t see the future for pharma supply chains, but we can know it’s going to have to be a lot more transparent.